Copy link
Aortic Stenosis: Etiology, Pathophysiology, and Clinical Presentation
Last updated: 06/13/2023
Key Points
- Aortic stenosis is defined as a narrowing of the aortic valve opening.
- Causes of aortic stenosis include calcific degeneration, rheumatic heart disease, or congenital bicuspid valve.
- The classic triad of late-stage symptoms includes syncope, exertional angina, and dyspnea and it has been associated with increased mortality.
Etiology
- Causes of aortic stenosis include calcific degeneration, rheumatic disease, or congenital bicuspid aortic valve (Figure 1).
- Calcific degeneration may be due to aging, inflammation, and lipid accumulation and is characterized by calcification originating at the tips of the aortic valve cusps.
- Rheumatic aortic stenosis is characterized by leaflet thickening and commissural fusion. There is often concomitant mitral valve involvement.
- Congenital aortic stenosis is a result of superimposed calcifications on a bicuspid aortic valve.1
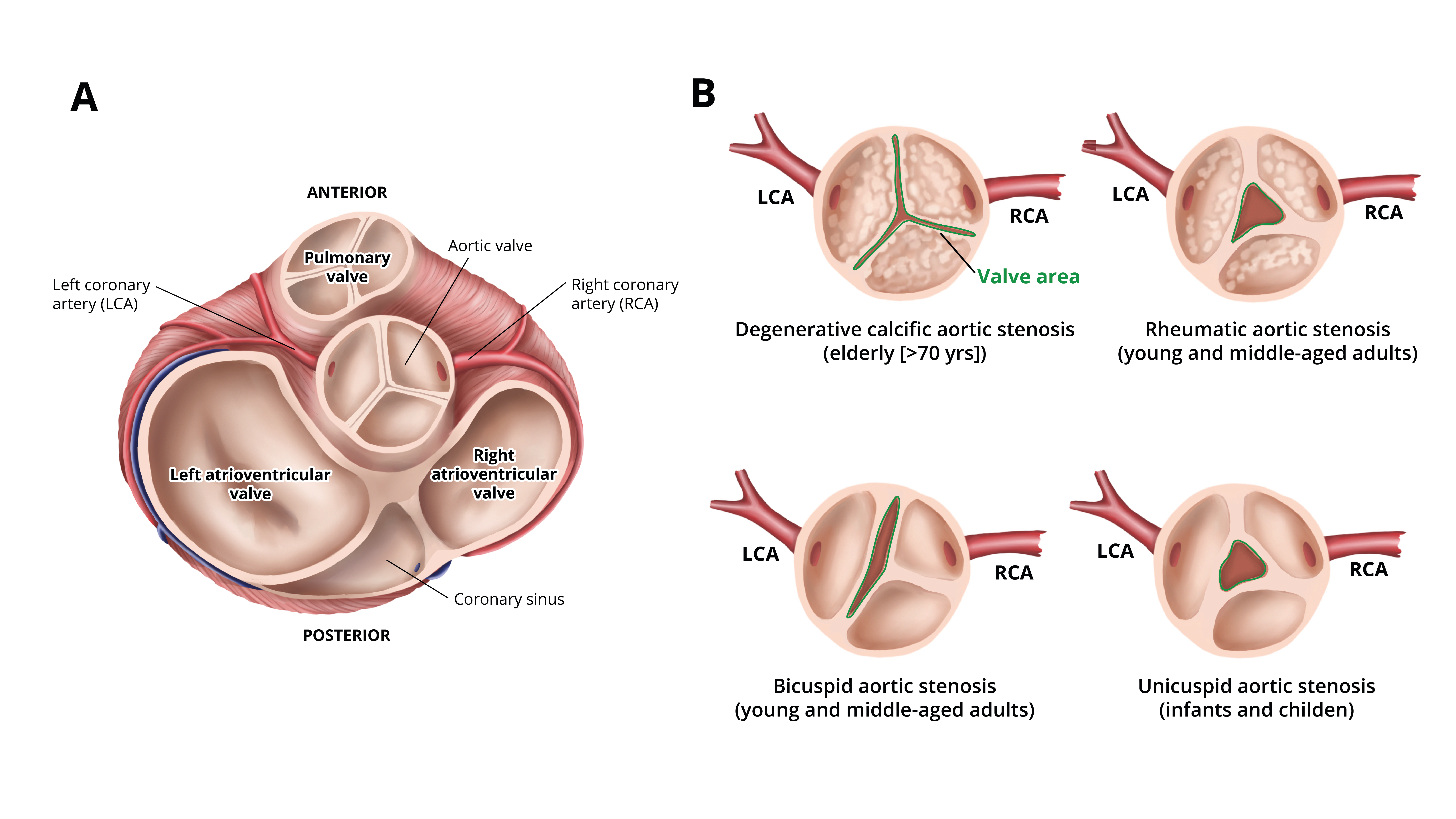
Figure 1. A: Normal aortic valve anatomy, B: Common causes of aortic stenosis. Redrawn from Manning WJ. JAMA. 2013;310(14): 1490-7.
Evaluation
- Echocardiography is the main method used to diagnose aortic stenosis and characterize severity (Figure 2).2 Both transthoracic and transesophageal echocardiography may be used.
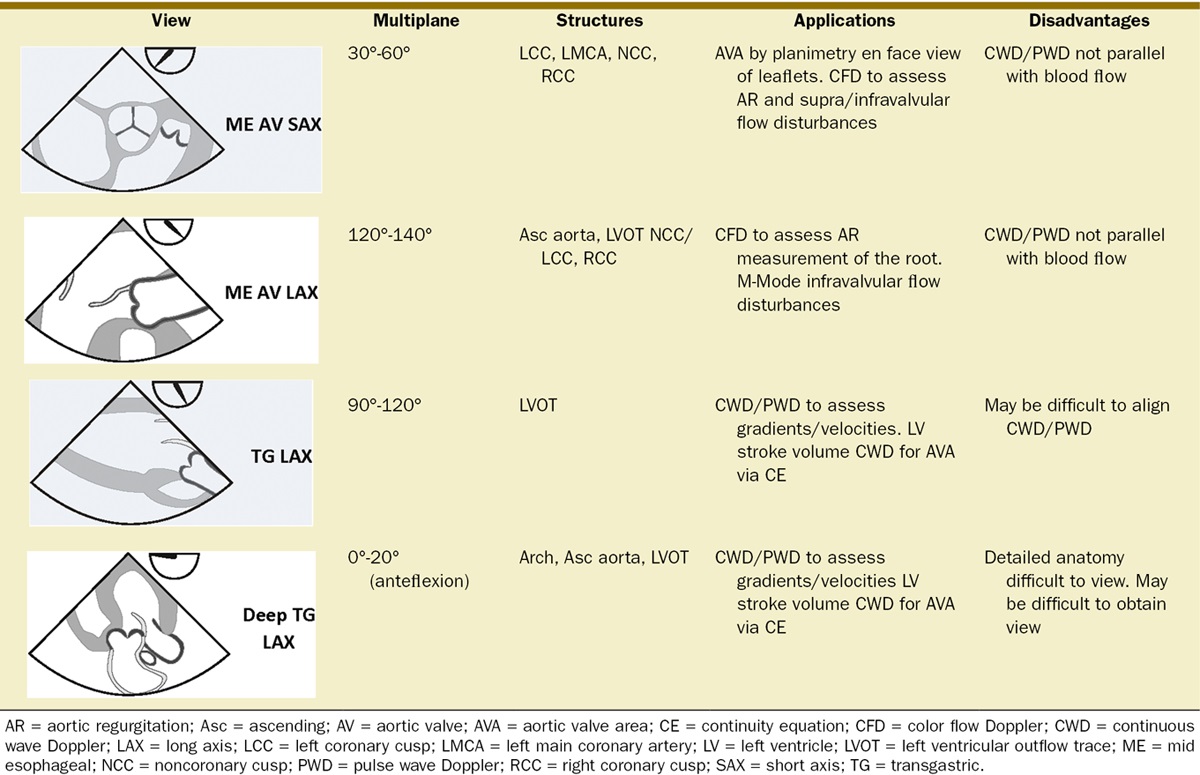
Figure 2. The four basic views of the aortic valve on transesophageal echocardiogram. Used with permission from Roberts JD, et al. Aortic valve anatomy and assessment by transesophageal echocardiography. Anesth Analg. 2013;117(6):1286-90.2
- Doppler echocardiography can be used to determine the pressure gradient and jet velocity across the aortic valve, as well as aortic valve area.1,3
- The continuity equation can be used to calculate aortic valve area, while the peak pressure gradient is estimated from the peak velocity (Figure 3).2
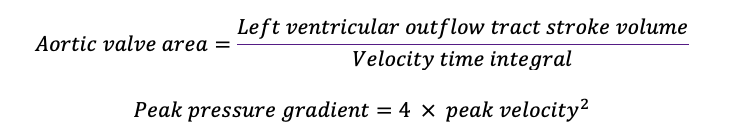
Figure 3. Equations for aortic valve area and peak pressure gradient.2
- The severity of aortic stenosis is determined by aortic valve jet velocity, mean pressure gradient, and aortic valve area (Table 1).1,3
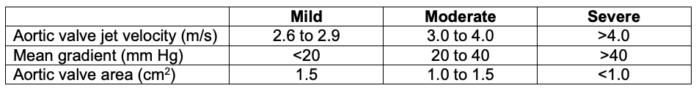
Table 1. Grading of aortic stenosis severity. Adapted from von Homeyer, et al. Aortic stenosis: Echocardiographic diagnosis. Anesth Analg. 2012;115(3):517-21.1
- Multidetector computed tomography to evaluate calcium score and cardiac catheterization to evaluate gradients may be used for diagnosis when history, presentation, and echocardiographic findings are inconclusive for aortic stenosis.3,5
Epidemiology
- Aortic stenosis is the most prevalent valvular disease in developed countries.4 Rheumatic aortic stenosis is more commonly seen in developing countries.1
- The prevalence of critical aortic stenosis increases with age, from 1% to 2% in patients 75 to 76 years of age to 6% in patients 85 to 86 years of age.3
- Aortic stenosis affects up to 10% of the population by the eighth decade.1
- The annual mortality of severe aortic stenosis is 25%, with an average survival of 2 to 3 years after symptom onset.3,5
- Calcific aortic stenosis presents in older patients. One study showed that 9% of aortic valve sclerosis patients progressed to calcific aortic stenosis.3
- Congenital aortic stenosis is often seen in young adults. With a prevalence of 0.5% to 2%, bicuspid aortic valve is the most common congenital heart disease. Sixty percent of patients with bicuspid aortic valve who undergo aortic valve replacement for severe aortic stenosis are younger than 70 years of age.3
Pathophysiology
- Calcific aortic stenosis is caused by inflammation due to endothelial damage from mechanical stress, fibrosis, leaflet thickening, and calcification.5
- Leaflet stiffness in calcific aortic stenosis leads to a narrower aortic valve and an increased pressure gradient across the aortic valve.5
- Decreases in aortic valve area beyond half of the normal valve area results in greater left ventricular pressure overload, which leads to compensatory left ventricular hypertrophy and impaired diastolic function.
- If left untreated, aortic stenosis is fatal. Severe aortic stenosis results in reduced left ventricular ejection fraction, which leads to decreased stroke volume.5
Clinical Presentation
- In the early stages of aortic stenosis, most patients are asymptomatic due to physiologic compensation via left ventricular hypertrophy.
- Early symptoms of aortic stenosis include shortness of breath and decreased exercise tolerance.3
- Late symptoms include the classic triad of
- exertional angina — when the myocardial oxygen demand exceeds the supply;
- syncope — due to the inability of the heart to increase stroke volume in response to increased exertion or decreased peripheral vascular resistance; and
- dyspnea from heart failure.
- This presentation portends a worse disease course than the asymptomatic patient.4
- Patients with aortic stenosis are at an increased risk for sudden death from ventricular arrhythmias.
- Physical exam findings include a mid to late systolic murmur at the right upper sternal border, delayed and reduced carotid upstroke (pulsus parvus et tardus), and decreased second heart sound.3
References
- Von Homeyer P, Oxorn DC. Aortic stenosis: Echocardiographic diagnosis. Anesth Analg. 2012;115(3):517-21. PubMed
- Roberts JD, Dhawan R, Chaney MA, et al. Aortic valve anatomy and assessment by transesophageal echocardiography. Anesth Analg. 2013;117(6):1286-90. PubMed
- Kanwar A, Thaden JJ, Nkomo VT. Management of patients with aortic valve stenosis. Mayo Clin Proc. 2018;93(4):488-508. PubMed
- Carabello BA, Paulus WJ. Aortic stenosis. Lancet. 2009;373(9667):956-66. PubMed
- Joseph J, Naqvi SY, Giri J, et al. Aortic Stenosis: Pathophysiology, diagnosis, and therapy. Am J Med. 2017;130(3):253-63. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.