Copy link
Ocular Trauma
Last updated: 01/20/2023
Key Points
- Commonly used anesthetic drugs can cause transient increases in intraocular pressure.
- The primary anesthetic goals for emergency ocular surgery are providing profound analgesia and preventing increases in intraocular pressure.
Epidemiology
- The most common type of ocular trauma is a foreign body in the eye, which accounts for about 35% of all ocular injuries.
Open wounds or contusions from blunt ocular trauma each account for about 25% of all ocular injuries.
Anesthetic Goals for Emergency Ocular Surgery1,2
- Provide a stationary globe
- Provide profound analgesia
- Monitoring and attenuation of the oculocardiac reflex
- Prevent harmful increases in intraocular pressure (IOP) by limiting coughing, retching, vomiting, forceful blinking, or crying during emergence
- It is especially important to limit increases in IOP in open globe injuries as elevated IOP increases the risk of extrusion of ocular contents.
Factors Affecting Intraocular Pressure
- IOP is defined as the pressure exerted by the contents of the eye against its containing wall.
- IOP is essential to maintain the refractive properties of the eye, and elevated IOPs reduce the perfusion of ocular structures such as the retina.2
- Normal IOP is 11-21 mm Hg, with cyclic fluctuations of 2-3 mm Hg throughout the day.2 IOP above 24 mm Hg is considered pathologic.2
- An increase in IOP reduces the perfusion of ocular structures in a linear manner. An acute increase in IOP of the order of 20 mm Hg over 5 minutes reduces blood flow to the retina and may interfere with the delivery of essential neurotrophins from the brain to the retina.
- Acute reduction in IOP can cause loss of visual acuity and retinal detachment.
- The principal physiological factor affecting IOP is the balance between aqueous humor production and outflow rates. Other factors affecting IOP include neural regulation of extraocular muscle tone, and episcleral venous pressure via its effect on aqueous humor outflow and choroidal blood volume.
- Mean ocular perfusion pressure (MOPP) = mean arterial pressure (MAP) in the ophthalmic artery minus the IOP or ocular venous pressure, whichever is highest. In the sitting or standing position, the MAP in the ophthalmic artery is approximately two-thirds of the brachial artery pressure. Therefore, MOPP = 2/3 MAP (measured at brachial or radial artery) minus IOP. The normal MOPP range is 45-55 mm Hg, with nocturnal reductions of 10-20%.2
- During general anesthesia, the most significant increases in IOP occur during laryngoscopy and emergence.
- The effect of commonly used anesthetic drugs on IOP is discussed in the sections below.
- Supine, prone, and steep Trendelenburg positioning increases IOP by reducing venous drainage resulting in decreased aqueous drainage.
- Positive end-expiratory pressure (PEEP) less than 15 cm H2O does not appreciably increase IOP.
- The table below lists the effects of physiological and perioperative factors affecting IOP.
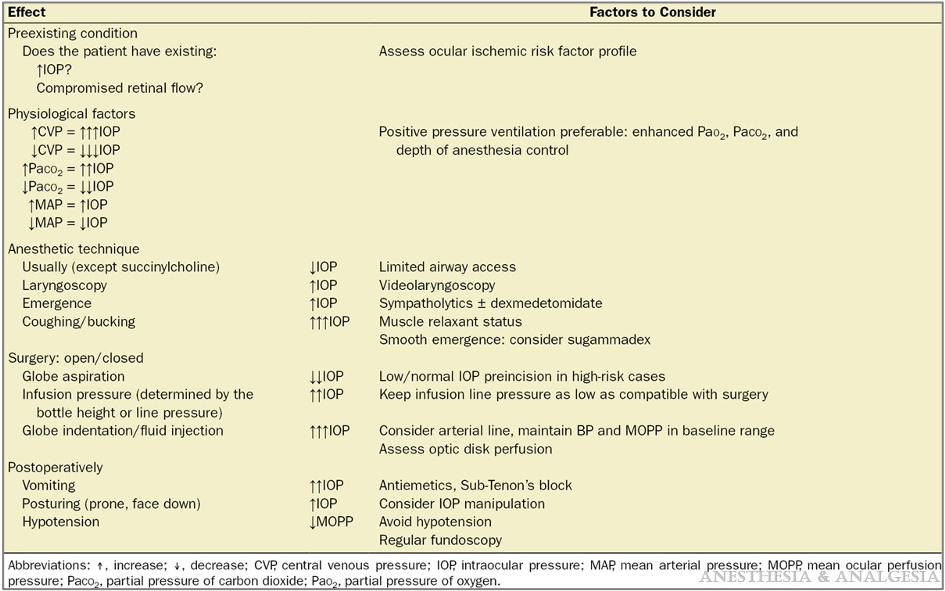
Table 1. Physiological and perioperative factors affecting IOP. Reproduced with permission from Kelly DJ, Farrell SM. Physiology and Role of Intraocular Pressure in Contemporary Anesthesia. Anesth Analg. 2018;126(5):1551-62.2
Choice of Anesthetic
- General anesthesia is the most common choice, especially for open globe injuries.
- Topical or regional anesthesia can be considered if difficult laryngoscopy or intubation is anticipated.
General Anesthesia1,2
- Premedication with 1-2 mg intravenous (IV) midazolam does not affect IOP and can be helpful in relieving preoperative anxiety. Premedication with IV dexmedetomidine 0.2-0.8 mcg/kg administered over 10 minutes helps to prevent a significant increase in IOP during laryngoscopy.
- Standard ASA monitors must be used. The need for additional monitors depends on the patient’s comorbidities.
- Airway considerations include positioning the patient’s head up to minimize the risk of aspiration, and preoxygenation with 100% oxygen to increase the oxygen reserve.
- IV lidocaine 1-1.5 mg/kg can be administered two minutes before induction to minimize the increase in IOP caused by laryngoscopy.
- Rapid sequence induction and intubation is the preferred method of induction of general anesthesia for emergency ocular surgery, especially for an open globe injury.
- Inhaled anesthetics (e.g., sevoflurane), hypnotics (e.g., propofol), opioids (e.g., fentanyl) all lower IOP and are combined with a neuromuscular blocking agent for the maintenance of general anesthesia.
- While succinylcholine is associated with a small increase in IOP, there are no published reports of extrusion of ocular contents when it is administered along with an adequate dose of an anesthetic induction agent. Succinylcholine has the advantage of fast onset with a brief duration of action and provides excellent intubating conditions. Alternatively, a relatively larger dose of a nondepolarizing neuromuscular blocking agent (e.g., 1.2 mg/kg rocuronium) can be used along with an anesthetic induction agent to quickly achieve intubating conditions without increasing IOP. If an unanticipated difficult airway is encountered, sugammadex can be administered to rapidly reverse the effects of rocuronium.
- An alternative technique for induction without the use of neuromuscular blocking agents is to utilize remifentanil. Administration of remifentanil 3-5 mcg/kg along with propofol 2-2.5 mg/kg provides excellent intubating conditions after 1-2.5 minutes. Typically, ephedrine 10 mg is coadministered to avoid profound bradycardia and hypotension that may develop with this combination of induction agents.
- Endotracheal tube (ETT) is preferred over laryngeal mask airway (LMA) due to limited intraoperative airway access in ocular surgeries despite lower sympathetic response and a lower increase in IOP with LMA over ETT.
- Video laryngoscopy appears to produce a lower increase in IOP compared to direct laryngoscopy.2
- After intubation, a deep plane of anesthesia is maintained during surgery to prevent movement and coughing.
- Inhaled anesthetic agents such as sevoflurane or desflurane are often used as they decrease production and increase the flow of aqueous humor, resulting in the lowering of IOP and decreasing extraocular tension.
- For patients at high risk for postoperative nausea and vomiting (PONV), total IV anesthetic (TIVA) with propofol should be considered as it is important to avoid the increase in IOP that can occur with PONV.
- For emergence from anesthesia, it is important to prevent coughing, retching, and vomiting as these increase IOP significantly. Prophylactic antiemetics (e.g., ondansetron 4 mg) should be administered prior to emergence from anesthesia. Administration of IV lidocaine 1-2 mg/kg prior to extubating may attenuate coughing but may prolong the time to awakening.
- For reversal of neuromuscular blockade, sugammadex is preferred over neostigmine/glycopyrrolate as it minimizes elevation of IOP after tracheal extubation.2
- If the patient has appropriately fasted prior to general anesthesia and has a reassuring airway, extubating the patient while deeply anesthetized can avoid coughing and the resultant increase in IOP.
Anesthetic Drugs to Avoid
- Etomidate is relatively contraindicated in emergent ocular surgery as it may induce myoclonus severe enough to increase IOP.
- Ketamine was thought to be contraindicated for emergent ocular surgery as it may increase IOP due to its sympathomimetic effects. However, recent evidence has refuted the belief that ketamine increases IOP.2 However, ketamine can cause nystagmus and blepharospasm and adversely affect surgical conditions.
- Nitrous oxide should be avoided in ocular surgeries if there is a recent or planned injection of gas to create an intraocular bubble to internally tamponade a detached retina or if there is a concern for a vascular air embolism or pneumothorax.
Regional Anesthesia
- Options for regional anesthesia in ocular surgery include retrobulbar or peribulbar blocks. These are contraindicated in cases with penetrating eye injury as local anesthetic injection in such cases may increase IOP and increase the risk of extrusion of ocular contents. In general, regional anesthetic techniques are extremely challenging to perform in patients with ocular injuries due to the distortion of anatomy.
- In select cases, regional anesthesia may be a viable option for open globe injuries in the cornea, limbus, and areas in the globe less than 5 mm posterior to the limbus.
- In cases where salvaging vision is not likely, regional anesthesia may be preferred in patients with a difficult airway.
Difficult Airway
- In patients with a difficult airway and if regional anesthesia is not a viable option for ocular surgery, an awake fiberoptic intubation may be the safest option. To minimize the risk of increased IOP, periprocedural sedation for intubation is used with either a remifentanil or dexmedetomidine infusion or bolus doses of fentanyl, midazolam, and/or propofol. Additionally, topical anesthesia of the airway and nerve blocks that anesthetize the nasopharynx, oropharynx, glottis, and trachea are needed to keep IOP from increasing during intubation.
References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.