Copy link
Perioperative Sinus Tachycardia
Last updated: 04/06/2023
Key Points
- Sinus tachycardia is defined as sinus rhythm greater than 100 beats per minute (bpm).
- It is the most common atrial tachycardia during anesthesia and surgery.
- Sinus tachycardia is often a normal physiological response to a demand for greater cardiac output or increased sympathetic stimulation.
Introduction
- Sinus tachycardia is a rhythm in which the cardiac impulse arises from the sinoatrial node at a rate greater than 100 bpm.1 In children, the normal range for heart rate varies with age. Sinus tachycardia is usually less than 180 bpm in children and 220 bpm in infants.
- Sinus tachycardia is often a normal physiological response to a demand for greater cardiac output, increased sympathetic stimulation, or, less commonly, parasympathetic withdrawal.1
- Sinus tachycardia is the most common atrial tachycardia during anesthesia and surgery.2
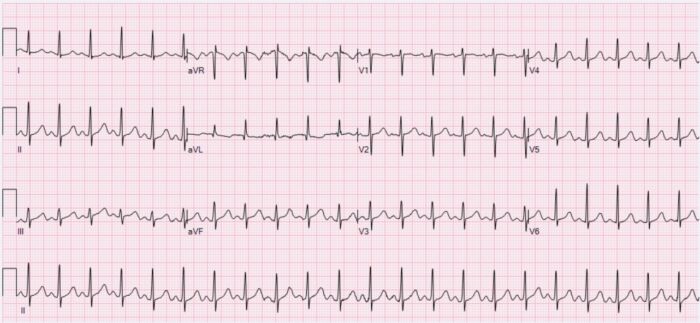
Figure 1. Sinus tachycardia with a heart rate of 132 bpm. Source: Wikimedia Commons. Ewingdo. CC BY-SA 4.0. Link.
Causes
The causes of sinus tachycardia in the perioperative setting can be categorized as follows.2,3
Normal Physiological Response
- Anxiety or pain
- Sympathetic response to laryngoscopy and intubation
- Inadequate anesthesia during surgical incision or intense surgical stimulation
- Stimulation of airway reflexes during emergence and extubation
Physiological Response to Maintain Cardiac Output and Oxygen Delivery
- Fever
- Hypovolemia
- Sepsis and other shock states
- Anemia
- Hypoxemia
- Hypercarbia
- Hypoglycemia
- Anaphylaxis
- Seizures
- Hyperthyroidism
- Malignant hyperthermia
- Pheochromocytoma
- Acute coronary ischemia and myocardial infarction
- Pericarditis
- Pericardial tamponade
- Pulmonary embolism (blood, air, fat, etc.)
Drugs
- Anticholinergics (atropine, glycopyrrolate)
- β2-agonists (albuterol, terbutaline)
- Ketamine
- Desflurane
- Inotropic agents
- Pancuronium
- Stimulants (nicotine, caffeine)
- Illicit drugs (cocaine, amphetamine)
Iatrogenic
- During central line placement
- Bladder distension (blocked foley catheter)
- Pacemaker malfunction
- Endotracheal tube abutting carina.
Clinical Presentation
- Most patients with sinus tachycardia have signs and symptoms of the underlying condition (pain, fever, shortness of breath, etc.) rather than the tachycardia itself.1 Some patients may complain of palpitations and chest discomfort. Infants and young children may present with irritability and poor feeding.
- Tachycardia may result in
- decreased cardiac output due to shortened ventricular filling time;
- increased myocardial oxygen consumption; and
- reduced coronary blood flow.
Management
The management of perioperative sinus tachycardia is summarized in Table 1.2,3
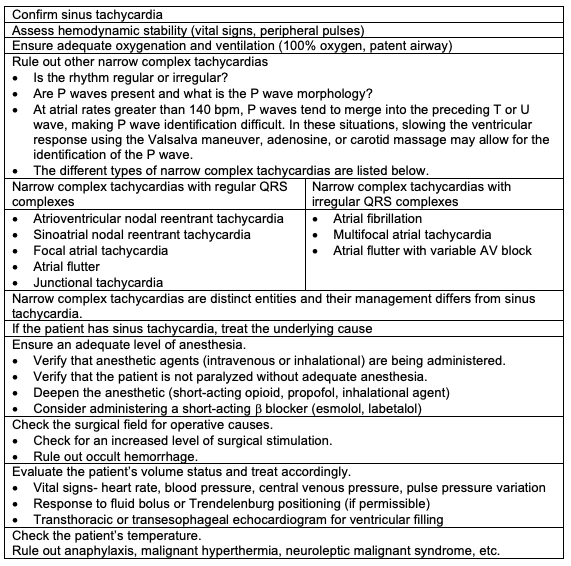
Table 1.
References
- Homoud MK. Sinus tachycardia: Evaluation and management. In: Post T, ed. UpToDate; 2023. Accessed February 18th, 2023. Link
- Methangkool E, Mahajan A. Arrhythmias during anesthesia. In: Post T, ed. UpToDate; 2023. Accessed February 18th, 2023. Link
- Kuan C, Pukenas EW. Sinus tachycardia in the pediatric patient. In: Gaba, DM, Burden AR, Howard SK, Fish KJ. Crisis Management in Anesthesiology. 2nd Edition. Philadelphia, PA. Elsevier/Saunders; 2015: 389-93.
- Panchal AR, Bartos JA, Cabańas JG, et al. Part 3: Adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142: S366-468. PubMed
- Topjian AA, Raymond TT, Atkins D, et al. Part 4: Pediatric basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142: S469-523. PubMed
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.