Copy link
Temperature Regulation in Pediatric Anesthesia
Last updated: 06/13/2023
Key Points
- Compared to adults, children and neonates have a larger surface area per kilogram, which has implications for temperature control.1,2
- The primary means that neonates produce heat is called nonshivering thermogenesis (metabolism of brown fat).1,2,4,5
- Temperature is regulated by the hypothalamus.3
- Hypothermia is associated with coagulopathy, delayed emergence from anesthesia, cardiac arrhythmias, respiratory depression, delayed wound healing and can be reduced by proper planning and monitoring.1,2,4
Introduction
- Temperature management is of utmost importance in anesthetized patients, particularly in children and neonates.
- Temperature regulation to thermal disturbances is determined by both central and skin temperatures.
- The hypothalamus uses a negative feedback system to minimize changes from preset “normal” values (normal being around 37°C (98.6°F) varying plus or minus one degree depending on the time of day).3
- The primary methods of heat loss in the operating room are listed below (Figure 1).
- Radiation (39%) includes heat loss from exposed skin or body parts.
- Convection (34%) includes heat loss to air immediately surrounding the body.
- Evaporation (24%) includes heat loss from sweat, respiratory mucosa, bowel, and wound surfaces.
- Conduction (3%) includes heat loss via contact with a cooler object such as the operating room table or cold fluids.
- All methods of heat loss should be addressed while planning a safe anesthetic, especially in neonates and infants.4
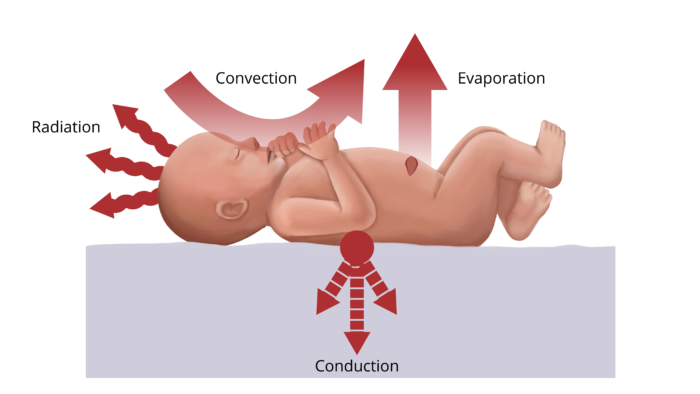
Figure 1. Primary methods of heat loss in the operating room.
Differences Between Children and Adults
Children vs. Adults
- Children and neonates, compared to adults, have thinner skin, low fat content, and a greater surface area relative to weight.1,2,4
- In adults, the primary responses to cold are shivering and arteriovenous shunt vasoconstriction, primarily in the extremities.6 In neonates, these systems are immature; therefore, they rely on nonshivering thermogenesis.
- Micro-preemies are very susceptible to hypothermia, particularly via evaporative heat loss and insensible fluid loss, as their epidermis has less keratin and little subcutaneous fat for insulation.4
- Close temperature monitoring in neonates and infants is of great importance.
Nonshivering Thermogenesis (NST)
- Nonshivering thermogenesis (NST) is heat production due to metabolic energy transformation.
- It relies on brown fat and, to a lesser degree, also on skeletal muscle, liver, brain, and white fat and does not involve contraction of skeletal muscle.4,5
- Neonates produce heat through the metabolism of brown fat by shifting hepatic oxidative phosphorylation to a more thermogenic pathway.
- Brown fat is highly vascularized and rich in sympathetic innervation, primarily b-3 receptors which are triggered by norepinephrine during cold stress.
- Cold stress increases lipase activity in brown fat and results in the release of free fatty acids.4
- Therefore, the heat produced by NST is mainly a byproduct of fatty acid metabolism, and to a lesser extent, from glucose metabolism.5
- The substrate for NST is brown fat.
- In the human fetus, brown fat differentiates between 20 (or 26 weeks, depending on which source) to 30 weeks of gestational age and comprises only 2% to 6% of an infant’s total body weight.
- It is anatomically located between the scapulae, in small amounts around the blood vessels in the neck, larger deposits in the axillae, modest amounts in the mediastinum, around the internal mammary vessels, and around the adrenal glands or kidneys.4,5
- Brown fat gets its color from the high number of mitochondria, densely packed with cristae which allow for increased content of respiratory-chain components.5
- The cold infant compensates by shivering and NST. However, the ability to shiver is limited in infants younger than 3 months. Clinically significant NST is possible as soon as a few hours after birth and can persist until around 2 years of age.2,5
- NST is severely limited in premature infants and neonates whose fat stores are deficient.1,2,4,5
NST Inhibition and Stress
- Cold stress causes increased oxygen consumption and metabolic acidosis.2
- NST is inhibited by ganglionic and b-receptor blockade (ganglionic blockers cause vasodilation by blocking postganglionic acetylcholine receptors, preventing depolarization), volatile anesthetics, sedative-hypnotic agents (such as propofol and dexmedetomidine), and opioids in a dose-dependent manner.1,2,5,6
- Volatile anesthetics inhibit NST within 5 minutes of turning on the gas; this inhibition remains 15 minutes after the gas has been turned off.5
- Sympathectomy inhibits NST. Neuraxial anesthesia impairs central thermoregulatory control via a pharmacologic sympathectomy and reduces vasoconstriction and shivering thresholds proportional to block height.6
Effects of Hypothermia
- Heat loss from the head is quite significant in neonates and infants.2
- Heat loss can be worsened by:
- prolonged exposure to an inadequately warmed operating room;
- administration of room-temperature intravenous fluid;
- dehumidified gases; and
- the effects of anesthetic gases on temperature regulation, via peripheral vasodilation resulting in the redistribution of blood volume to the periphery.1
- Hypothermia has been associated with complications such as:
- coagulopathy
- impairs platelet aggregation via reduced release of thromboxane A3
- reduces the activity of all enzymes in the coagulation cascade, which reduces clot formation6
- delayed emergence from anesthesia
- delayed wound healing and infection
- reduces tissue perfusion to the wounded tissue and reduces access for key immune cells (macrophages)
- reduces motility of immune cells
- reduces scar formation, which is necessary to prevent wound dehiscence6
- cardiac arrhythmias/cardiac ischemia
- respiratory depression
- increased pulmonary vascular resistance
- altered pharmacodynamics1,6
- increases susceptibility to many drugs
- prolongs the action of several drugs used during an anesthetic, particularly neuromuscular blocking agents6
- coagulopathy
- Most cellular functions are temperature-dependent; hypothermia provokes systemic responses (e.g., reduction in drug metabolism due to impacts on proteins in CYP system, increased risk of surgical infection due to inhibition of immune function, and reduction in inflammatory responses).6
Warming Techniques/Devices
- It is important to plan ahead to reduce the risk of hypothermia in neonates and children.
- A warm operating room (26°C/80°F) will reduce heat lost by radiation.1,2,4
- A hot air mattress on the bed and turned on prior to the infant arriving in the room is the most effective means of keeping a micro-preemie normothermic.1,2,4
- Warmed intravenous and irrigation fluids, blood, surgical skin preparations, and heat lamps all help reduce heat loss.1,2,4
- During transport, it is important to keep the infant covered and warm.
- Other strategies include the use of humidified gases in the ventilator circuit, covering the head, and keeping the child’s skin dry (reduces evaporative heat loss).4
- Temperature should be carefully monitored in infants as overheating can easily occur.1,4
References
- Butterworth IV JF, Mackey DC, Wasnick JD. eds. Pediatric anesthesia. In: Morgan & Mikhail’s Clinical Anesthesiology, 7e. McGraw Hill; 2022.
- Gropper MA, Miller RD, Cohen NH, Absalom AR, Vutskits L, Davidson A. Chapter 77: Pediatric Anesthesia. In: Miller's Anesthesia. Elsevier; 2020:2420-58.
- Bissonnette B. Temperature monitoring in pediatric anesthesia. International Anesthesiology Clinics. 1992; 30 (4): 63-76. PubMed
- Cote CJ, Lerman J, Anderson BJ, Spaeth JP, Lam JE. The Extremely Premature Infant (Micropremie) and Common Neonatal Emergencies. In: Cote and Lerman's A Practice of Anesthesia for Infants and Children. Elsevier; 2019: 848-9.
- Luginbuehl I, Bissonette B, Davis PJ. Cladis FP, Motoyama EK. Eds. Thermoregulation: Physiology and perioperative disturbances. In: Smith’s Anesthesia for Infants and Children, 8e. Mosby; 2011.157-78.
- Sessler D. Perioperative temperature management. In: Post T, ed UpToDate. 2023. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.