Copy link
Postoperative Liver Dysfunction
Last updated: 01/27/2023
Key Points
- Postoperative liver dysfunction (POLD) is common after surgery, and jaundice (hyperbilirubinemia) is the most frequent sign.1
- Even healthy patients without prior history or symptoms of liver disease may exhibit abnormal liver function tests postoperatively.
- For patients with known underlying liver disease, postoperative jaundice occurs regularly and in severe cases, can lead to postoperative liver failure (POLF).
Introduction
- Bilirubin is a byproduct of the breakdown of heme from red blood cells. Under normal conditions, the liver conjugates the bilirubin to make it water-soluble and secretes it into the gastrointestinal tract as bile. Jaundice, which is the result of hyperbilirubinemia, occurs when there is a breakdown anywhere along the normal bilirubin uptake, metabolism, or excretion processes.
- The combined stresses of anesthesia and surgery frequently produce some degree of hepatic dysfunction, often manifested as jaundice. At the mildest end of the spectrum, the POLD is short-lasting and leads to a mild elevation in bilirubin and liver enzyme levels, while at the most severe end, a sustained deterioration in the metabolic and synthetic functions of the liver culminating in postoperative liver failure.
- The effects of anesthesia and surgery often result in a fall in hepatic blood flow leading to a reduction in O2 delivery, which can be as much as 30-40%.2 It is thought that ischemia and the subsequent reperfusion injury is responsible for much of the POLD reported.
Causes of Postoperative Jaundice
- It is useful to categorize the causes of jaundice and liver dysfunction into three main groups: prehepatic, intrahepatic, and posthepatic.3
- Prehepatic jaundice usually arises when the quantity of heme delivered to the liver surpasses its ability to conjugate it all.
- This presents as an unconjugated hyperbilirubinemia that resolves fully over time.
- In most cases, the excess heme is produced by hemolysis following bleeding during surgery or the use of blood transfusions.
- Intrahepatic jaundice is due to either the hepatocyte’s inability to conjugate bilirubin (hepatocellular dysfunction), or obstruction of the intrahepatic bile ducts resulting in a failure to transport the bile out of the liver (as in cirrhosis).
- It usually presents as an increase in both conjugated and unconjugated bilirubin.
- Hepatocellular dysfunction can be a result of hepatocyte failure from either ischemic or drug-induced stresses.
- “Shock liver” – acute ischemic hypoperfusion and subsequent reperfusion injury – is a severe condition reflecting massive damage to hepatocytes from ischemia. It leads to a large increase in the level of tissue transaminases along with a similar rise in the international normalized ratio, reflecting a deterioration in the synthetic functions of the liver. Exposure to a variety of hepatotoxic drugs can cause a similar picture, often developing in the days after surgery and improving after cessation of the offending drug (e.g., acetaminophen, inhaled volatile agents, amoxicillin/clavulanate, amiodarone).
- Posthepatic jaundice is usually secondary to the surgery itself (where damage to the biliary system often requires endoscopic intervention to aid resolution).
- This presents with an obstructive jaundice picture (conjugated hyperbilirubinemia with mildly elevated transaminases and alkaline phosphatase).
- A common example would be bile duct stenosis following liver transplantation.
- Postoperative jaundice is often multifactorial in origin (Figure 1, Table 1).
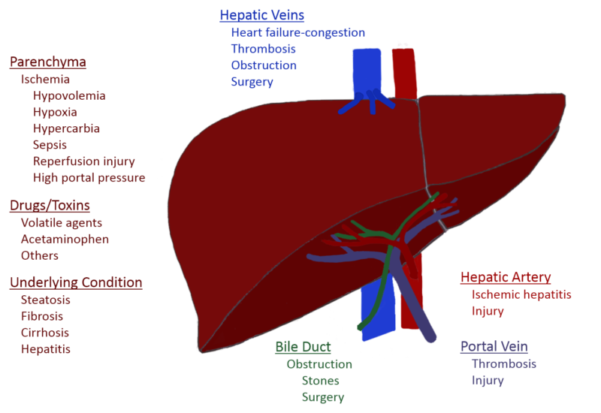
Figure 1. Causes of postoperative liver dysfunction (POLD)
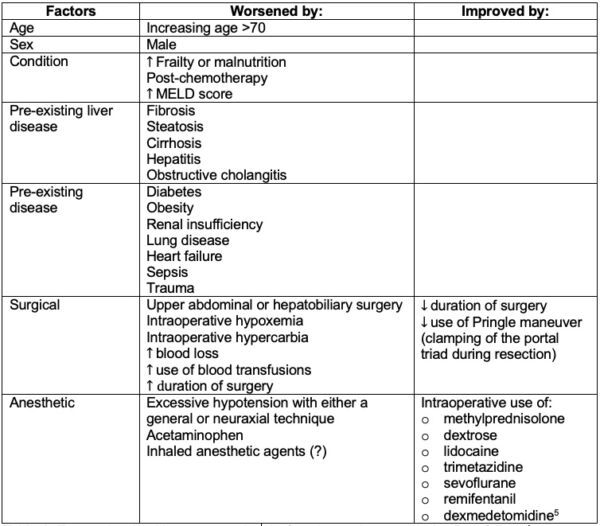
Table 1. Factors involved in postoperative dysfunction and postoperative liver failure.4
Prevention and Management
- Patients should be properly assessed and investigated before selection.
- The most appropriate anesthetic technique considering the patient’s pre-existing condition is important.
- Management of POLD should focus on treating the underlying cause.
- Frequent monitoring of blood tests may be necessary.
- Find alternatives for any potentially hepatotoxic drugs
- Seek specialized advice for potential surgical problems
- Supportive care is often the only option until the liver is able to self-repair.
References
- Faust TW, Reddy KR. Postoperative jaundice. Clin Liver Dis. 2004;8(1):151-66. PubMed
- Cowan RE, Jackson BT, Grainger SL, et al. Effects of anesthetic agents and abdominal surgery on liver blood flow. Hepatology. 1991;14(6):1161-66. PubMed
- Fink SA. Approach to the patient with postoperative jaundice. In: UpToDate, Brown R (Ed), UpToDate, Waltham MA (Accessed July 10, 2022).
- Pandey CK, Nath SS, Pandey VK, et al. Perioperative ischaemia-induced liver injury and protection strategies: An expanding horizon for anaesthesiologists. Indian J Anaesth. 2013;57(3):223-9. PubMed
- Huang YQ, Wen RT, Li XT, et al. The protective effect of dexmedetomidine against ischemia-reperfusion injury after hepatectomy: A meta-analysis of randomized controlled trials. Front Pharmacol. 2021; 12:747911. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.