Copy link
Carcinoid Syndrome
Last updated: 04/20/2023
Key Points
- Carcinoid syndrome (CS) is a paraneoplastic syndrome associated with neuroendocrine tumors that arise primarily from the gastrointestinal (GI) tract, and the lungs are the most common site of origin outside the GI tract.
- Serotonin is the primary substance released in carcinoid syndrome.
- The main symptoms of CS are episodic facial flushing, hypotension, tachycardia, diarrhea, bronchoconstriction, venous telangiectasia, dyspnea and ultimately fibrotic deposits, and carcinoid heart disease (CHD).
- Treatment is primarily focused on symptomatic relief with somatostatin analogs, such as octreotide and lanreotide.
Introduction
- Carcinoid syndrome (CS) is a paraneoplastic syndrome associated with the secretion of several humoral factors, such as polypeptides, vasoactive amines, and prostaglandins.1
- CS is predominantly associated with neuroendocrine tumors (NETs) that arise from the midgut, rectum, and ileum, in the setting of extensive liver metastases but may be present in patients with bronchial carcinoids and, more rarely, in patients with pancreatic NETs.2
- In patients with extensive liver metastases, many tumor-secreted substances are not completely metabolized by hepatic or pulmonary cells and enter the systemic circulation, causing carcinoid symptoms.2
- Carcinoid-produced substances may also enter the systemic circulation when a patient develops a foramen ovale or when the tumor is primarily located in the bronchi.3
- Patients with carcinoid syndrome present with vasomotor changes, hypermotility of the GI tract, hypotension, bronchospasm, and in cases of valvular involvement with symptoms and signs of heart failure.2
- CHD is the initial presentation of carcinoid syndrome in up to 20% of patients and occurs in more than 50% of these patients.4
Pathophysiology
- More than 40 substances have been identified as being potentially related to CS; however, their individual contributions in triggering different carcinoid symptoms and complications, such as CHD, remain unclear.5
- These substances include serotonin (5-HT), which appears to be the primary marker associated with the syndrome, as well as histamine, kallikrein, prostaglandins, and tachykinins.3
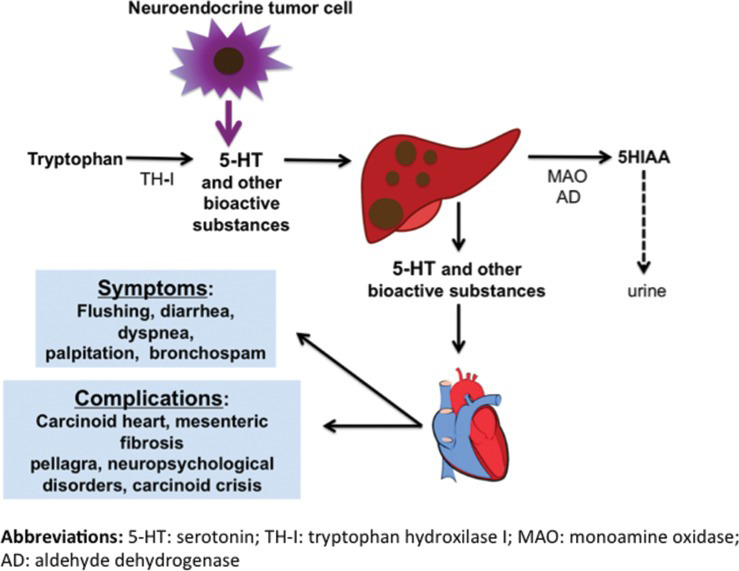
Figure 1. Pathophysiology of CS. Source: Ferrari AC, et al. Clinics. 2018;73(suppl 1): e490s.2 CC BY SA 4.0
- CHD has characteristic findings of plaque-like deposits of fibrous tissue. A carcinoid plaque is composed of smooth muscle cells, myofibroblasts, extracellular matrix, and an overlying endothelial layer. Fibrous deposits may involve the tricuspid valve, pulmonary valve, cardiac chambers, pulmonary artery, vena cava and coronary sinus. This can lead to stenosis and/or regurgitation of the valve, with regurgitation being more common.4
- Right-sided CHD is most common, owing to the biologically effective inactivation of humoral substances by the lung vasculature. However, left-sided involvement is seen in 5-10% of cases.4
- Left-sided CHD is usually associated with intracardiac shunting, extensive liver metastases, or bronchial carcinoid tumors.4
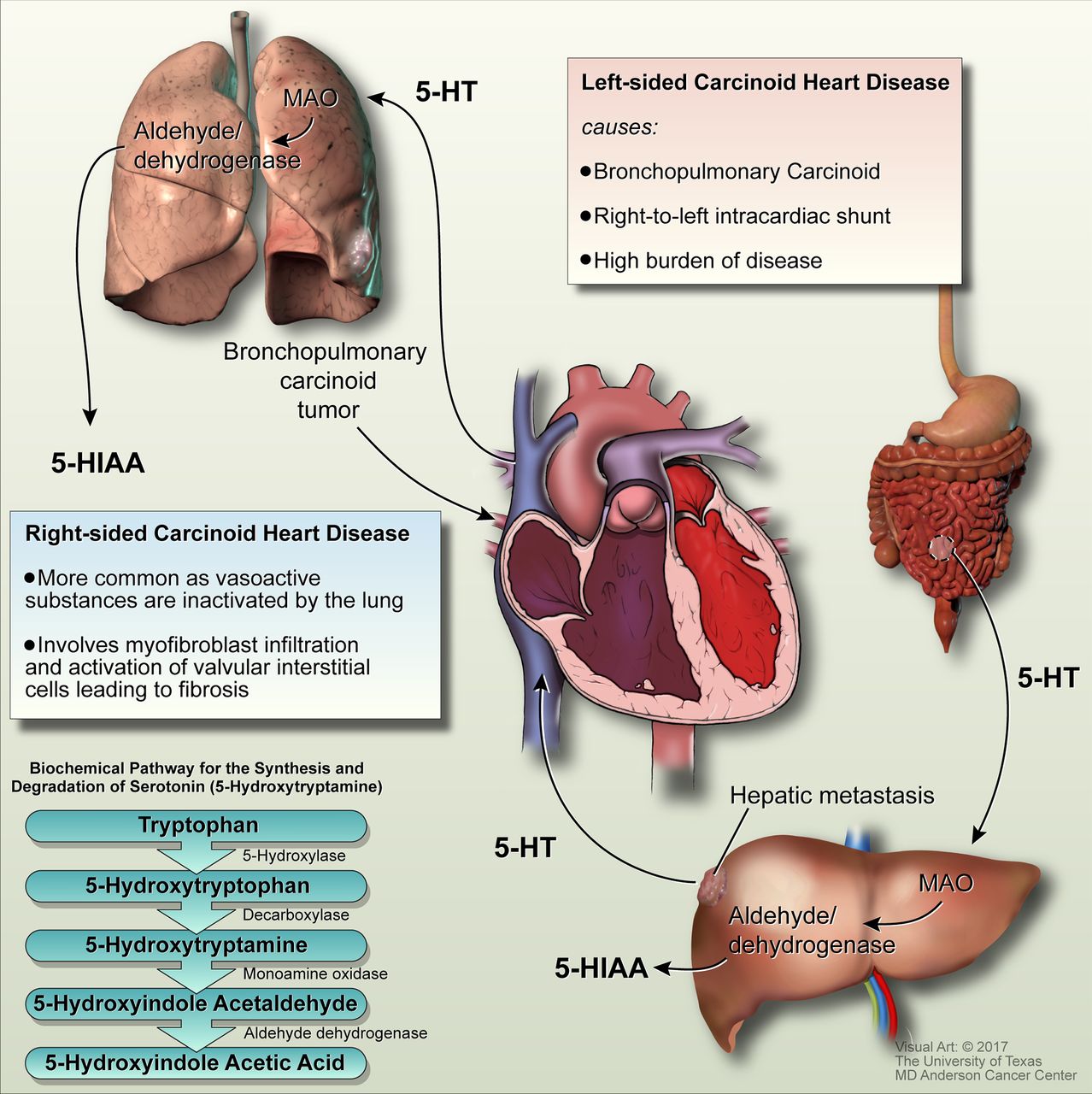
Figure 2. Systemic circulation of 5-hydroxytryptamine (5-HT) leading to CHD and the biochemical pathway for the synthesis and degradation of serotonin. 5-HIAA, 5-hydroxyindole acetic acid; MAO, monoamine oxidase. Used with permission from Hassan SA, et al. Heart 2017;103:1488–95.4
Clinical Presentation
- More than 75% of carcinoid tumors originate in the GI tract. The lung is the most common site of origin outside the GI tract. Tumors also have been reported in the genitourinary tract, thyroid, breast, pancreas, thymus, and liver.6
- Only 25% of carcinoid tumors produce mediators capable of causing symptoms of carcinoid syndrome. Normally the release of vasoactive substances causes little, if any, symptoms because the liver is able to rapidly inactivate these substances. With larger tumors, the liver’s ability to inactivate these substances may be overwhelmed, and CS results.6
- The main symptoms of CS are episodic facial flushing that may be accompanied by hypotension and tachycardia, diarrhea, bronchoconstriction, venous telangiectasia, dyspnea, and ultimately fibrotic complications such as mesenteric and retroperitoneal fibroses, and CHD.3
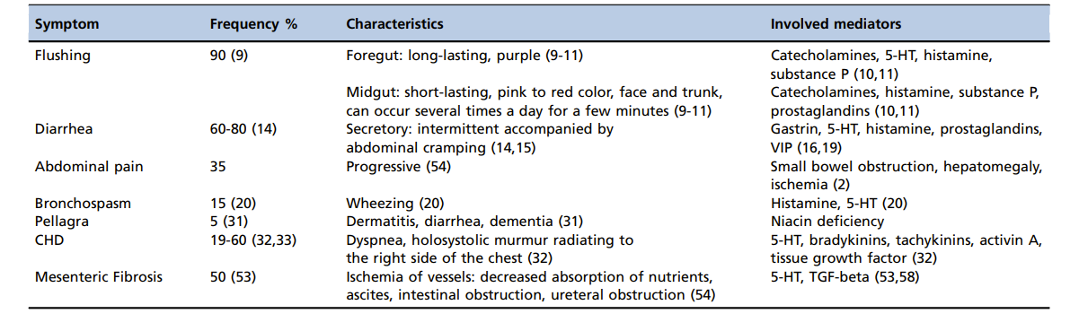
Table 1. Symptoms and signs of carcinoid syndrome. Source: Ferrari AC, et al. Clinics. 2018;73(suppl 1):e490s.2 CC BY SA 4.0.
- The classical presentation in CHD is a right-sided valvular lesion caused by fibrous tissue growth within the endocardium. Due to retraction and fixation of the valves, tricuspid regurgitation is a nearly universal finding; however, tricuspid stenosis, pulmonary insufficiency, and pulmonary stenosis may be found as well.6
- Structural valvular lesions can lead to symptomatic right-sided heart failure (edema, hepatomegaly, fatigue with exertion, and low cardiac output). Fibrous tissue growth, caused by carcinoid secretion of serotonin, may also interrupt electrical pathways, leading to arrhythmias. In addition to right-sided lesions, cardiac involvement may include left-sided lesions, myocardial metastases, and pericardial effusions.7
- If a bronchial tumor is present, left-sided heart lesions, pulmonary hypertension, and bronchospasm may result.6
- A life-threatening form of CS, known as carcinoid crisis, may be precipitated by physical manipulation of the tumor (including bedside palpation), chemical stimulation or tumor necrosis resulting from chemotherapy, and hepatic artery ligation or embolization. It may occur spontaneously or during the induction of anesthesia.6
- Clinical manifestations of carcinoid crisis include severe flushing with associated dramatic changes in blood pressure, cardiac arrhythmias, bronchoconstriction, and mental status changes.8
Diagnosis
- Serotonin is the most common mediator secreted by carcinoid tumors. Therefore, the most common test used to diagnose carcinoid tumors is the 24-hour urinary 5-hydroxy indole acetic acid (HIAA) assay which monitors the metabolite of serotonin. Normal levels of 5-HIAA are less than 10 mg in a 24-hour urine sample. Levels greater than 25 mg per 24 hours are considered diagnostic; however, up to 20% of carcinoid patients have normal urinary 5-HIAA levels. During the test, patients must avoid serotonin-rich foods such as bananas, avocados, plums, tomatoes, pineapples, kiwis, eggplant, plantain, and walnuts.6
- Various imaging techniques, including endoscopy, endoscopic ultrasound, and video capsule endoscopy, may be used to locate the tumor. Abdominal ultrasound computed tomographic (CT) scans, magnetic resonance imaging (MRI), selective mesenteric angiography, and barium small bowel radiography are all used to identify the primary tumor and, if possible, any metastases. Abdominal ultrasonography is quick and inexpensive, but it lacks reproducible sensitivity and specificity. MRI has been particularly useful in evaluating lesions of the lungs and liver.6
- Chromogranin A (CgA) is a protein found in most neuroendocrine cells and, when detected in plasma, it may be used as a general marker for carcinoid tumors, even those that are “non-functional.”6
- The pentagastrin challenge test may be used in conjunction with urinary 5-HIAA levels for the diagnosis and treatment of CS. This test utilizes the ability of gastrin to stimulate the release of other bioactive substances.6
- Chest radiography and electrocardiography (ECG) are often nonspecific and, thus, in patients with known CHD, echocardiography is used to evaluate the severity of cardiac lesions. However, chest radiography and bronchoscopy are often useful in diagnosing patients with suspected bronchial carcinoids.6
Treatment
- Treatment of patients with CS is aimed at symptomatic relief, delaying the progression of the disease, and improving survival.
- The main pillar of treatment for CS is the use of somatostatin analogs, such as octreotide and lanreotide. Approximately 80% of well-differentiated tumors express somatostatin receptors in the NET cell surface.2
- Octreotide and lanreotide bind to somatostatin receptors and inhibit the secretion of several hormones and vasoactive substances, thus improving flushing and diarrhea symptoms in over 80% of patients with CS.10
- The treatment of CHD includes the management of heart failure, treatment of the NE tumor, reduction in the production of related hormones (with the use of somatostatin analogs), and heart valve repair surgery.2
- Telotristat ethyl, a tryptophan hydroxylase inhibitor, decreases the production of serotonin; thus, reducing the levels of 5-HIAA in 24-hour urine tests. It is a promising treatment to prevent or delay the onset of CHD.2
- Valve surgery for CHD should be considered in symptomatic patients with controlled CS. Furthermore, operation early in the onset of cardiac symptoms is preferable, as a delay can result in the worsening of right-sided heart failure and increases the risk of surgery. Patients with progressive fatigue, worsening exercise capacity and declining RV function in the presence of controlled metastatic disease should be evaluated for valve surgery.4
- In right-sided CHD, Tricuspid valve replacement is the operation of choice. The use of valve prostheses requires thoughtful discussion and careful patient selection.4
Perioperative Management
- Surgery for carcinoid tumors is considered in appropriate patients for symptom control and palliation. Locoregional surgery, cytoreductive therapy for hepatic disease, radiofrequency ablation and hepatic arterial therapy have been used in the surgical management of carcinoid tumors.4
- The primary goals during the perioperative period are to prevent the release of bioactive mediators by avoiding factors that trigger the release of these bioactive mediators, thereby avoiding a carcinoid crisis.6
- The introduction of octreotide has rendered obsolete most of the literature concerning anesthesia for CS prior to that time.6
- Tumor-debulking surgery to reduce tumor size, hepatic artery embolization to reduce tumor size, biotherapy (e.g., interferon for tumor shrinkage), and chemotherapy for systemic spread can all stimulate release of vasoactive substances from tumor cells.6
Preoperative Management
- Preoperative assessment should include a history and physical examination that is focused on determining the presence and severity of any symptoms of CS, such as flushing, diarrhea, bronchospasm, and valvular heart disease.6
- Laboratory tests should include the standard chemistry, blood count, liver function panel, blood glucose concentration, ECG, type and screen, and urinary 5-HIAA measurements.6
- Premedication with benzodiazepines and antihistamines is useful in decreasing anxiety and stress.
- Octreotide can be given subcutaneously for symptomatic relief and for the prevention of perioperative hypotension.6
Intraoperative Management
- Rapid changes in blood pressure are often seen in carcinoid patients; therefore, in addition to standard monitors, invasive monitoring is recommended. An arterial catheter is indicated prior to the induction of anesthesia since the hypotension commonly seen with induction agents may trigger a carcinoid crisis.6
- In patients with coexisting cardiac dysfunction, monitoring of left ventricular function with a pulmonary artery catheter may be useful; however, in patients with right-sided cardiac involvement or valvular disease, transesophageal echocardiography may be more beneficial.6
- Care should be taken on induction to avoid catecholamine release. Propofol, thiopental sodium, and etomidate have been used to induce anesthesia; however, propofol has a more profound effect in suppressing the sympathetic response to intubation and thus may be the best induction agent in patients with carcinoid syndrome.10
- The use of succinylcholine has been debated because increases in intraabdominal pressure from fasciculations may trigger mediator release.6
- For pain management, opioids that are not associated with histamine release should be used.
- For maintenance, a balanced technique that incorporates positive pressure ventilation, an inhalation agent, a nondepolarizing neuromuscular blocking agent, and an opioid, most commonly fentanyl can be used. Nitrous oxide is safe as well.6
- Patients often have chronic right ventricular (RV) valvular lesions and heart failure; therefore, anesthetic factors that increase RV work with potential precipitation of acute RV failure should be avoided. Additionally, hypoxemia, hypercarbia, and light anesthesia should be avoided.6
- Due to concern for carcinoid crisis, an octreotide infusion (up to 300 g/hour) may be required and is continued for up to 48 hours after surgery. Treatment with antihistamines to reduce flushing and bronchospasm and with corticosteroids to reduce bradykinin production have also been used.4
- Anesthesia management should also include tight glucose monitoring since octreotide is well known to antagonize several hormones, including insulin.4
- Epidural and spinal anesthesia have been used successfully in patients with carcinoid tumors undergoing noncarcinoid surgery; however, care must be taken to adequately evaluate and premedicate the patient as needed to avoid hypotension.6
Postoperative Management
- Patients must be monitored postoperatively for signs of tumor mediator release, especially since they may have a delayed recovery from anesthesia. This may require admission to an intensive care or acute care unit. The effects of carcinoid tumor mediators may continue after tumor removal, and undetected metastases may still secrete peptides.6
- Patients with high serotonin levels are prone to a prolonged recovery period following general anesthesia. Preoperative drug therapy such as octreotide should be continued and, if indicated, reduced slowly over the first week. Fluids and electrolytes should be monitored since large fluid shifts may occur during surgery.6
- Analgesia to prevent excess sympathetic activity and stress is very important. Intravenous opioids and regional anesthesia have been used with good results.6
- Symptoms of CS, such as bronchospasm, hypotension, and flushing can be treated successfully with octreotide as quickly as 15 seconds. Other drugs have been reported with variable success, including vasopressin and angiotensin.6
- Postoperative hyperglycemia from elevated serotonin levels should be monitored closely and treated with an insulin infusion.
References
- Grozinsky-Glasberg S, Grossman AB, Gross DJ. Carcinoid heart disease: From pathophysiology to treatment– ‘Something in the way it moves’. Neuroendocrinology. 2015;101(4):263-73. PubMed
- Ferrari AC, Glasberg J, Riechelmann RP. Carcinoid syndrome: update on the pathophysiology and treatment. Clinics. 2018;73(suppl 1): e490s. PubMed
- Mota JM, Sousa LG, Riechelmann RP. Complications from carcinoid syndrome: review of the current evidence. Ecancermedicalscience. 2016; 10:662. PubMed
- Hassan SA, Banchs J, Illiescu C, et al. Carcinoid heart disease. Heart. 2017; 103:1488–1495. PubMed
- Modlin IM, Kidd M, Latich I, et al. Current status of gastrointestinal carcinoids. Gastroenterology. 2005;128(6):1717-51. PubMed
- Mancuso, K, Kaye AD, Boudreaux JP, et al. Carcinoid syndrome and perioperative anesthetic considerations. J Clin Anesth. 2011; 23(4): 329-41. PubMed
- Pellikka PA, Tajik AJ, Khandheria BK, et al. Carcinoid heart disease. Clinical and echocardiographic spectrum in 74 patients. Circulation.1993; 87:1188-96. PubMed
- Kahil ME, Brown H, Fred HL. The carcinoid crisis. Arch Intern Med. 1964; 114:26-8. PubMed
- Vinik AI, Wolin EM, Liyanage N, et al. Evaluation of lanreotide depot/autogel efficacy and safety as a carcinoid syndrome treatment (ELECT): a randomized, double-blind, placebo-controlled trial. Endocr Pract. 2016;22(9):1068-80. PubMed
- Larsen R, Rathgeber J, Bagdahn A, et al. Effects of propofol on cardiovascular dynamics and coronary blood flow in geriatric patients. Anaesthesia. 1988(43 Suppl):25-31. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.