Copy link
Burn Injuries: Initial Evaluation and Management
Last updated: 01/12/2023
Key Points
- Major burns result in an inflammatory response characterized by an early burn shock phase followed by a hyperdynamic, hypermetabolic phase.
- Inhalation injuries may not be clinically evident immediately but are associated with significantly increased morbidity and mortality.
- Effective fluid resuscitation is crucial during the first 48 hours after burn injury, but excessive fluid administration can lead to pulmonary or airway edema.
Introduction
- Burns are traumatic injuries to the skin or other tissues that are primarily caused by heat or exposure to electricity, chemicals, friction, and radiation. Burn injuries are the fourth leading cause of trauma worldwide.1
- The American Burn Association estimates that there are approximately 450,000 burn-related emergency room visits each year, with 40,000 hospitalizations and 3,400 deaths.1
Burn Classifications
- Based on the depth of injury, burns are classified as superficial, superficial partial thickness, deep partial thickness, full thickness, and fourth degree burns (Table 1 and Figure 1).1
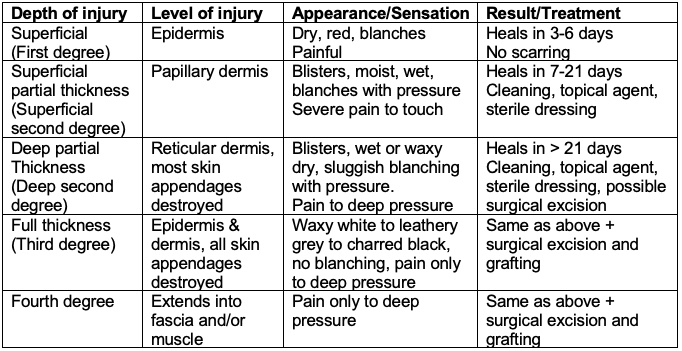
Table 1. Classification of burns by depth of injury. Adapted from Bittner EA, et al. Anesthesiology. 2015.1
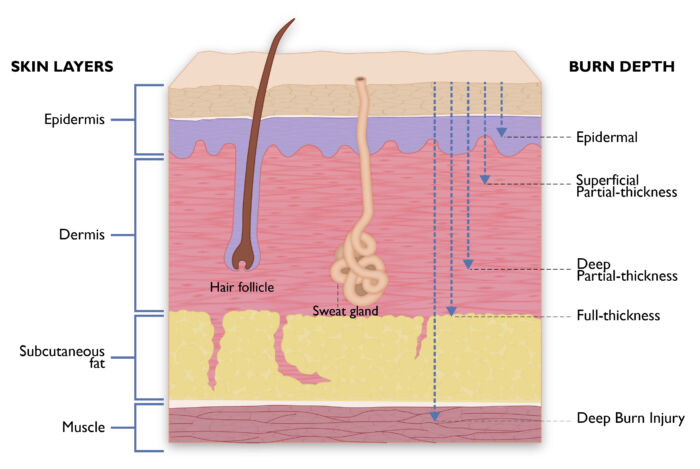
Figure 1. Classification of burns based on the depth of injury.
- Extent of Burns: percentage total body surface area (%TBSA) burns can be calculated using the Wallace Rule of Nines, Lund and Browder chart, or the palmar method.4 It is important to note that these %TBSA calculations only includes full-thickness and partial-thickness burns but not superficial-thickness burns.3
- Wallace Rule of Nines: This method is commonly used as it is simple and efficient to use. The %TBSA burns is calculated by dividing the body into percentages of 9 (Figure 2). This method is not accurate in children and obese patients.
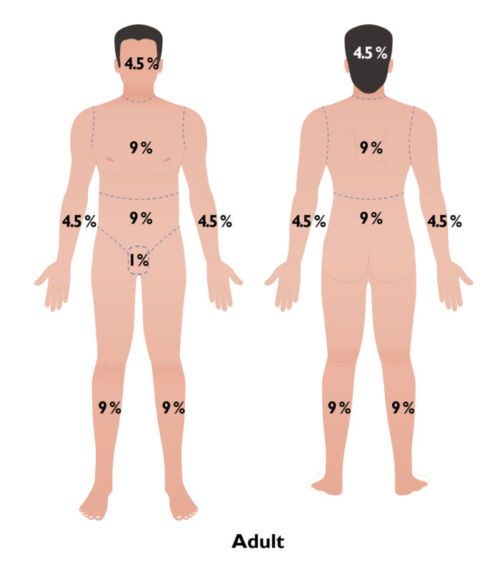
Figure 2. Rule of Nines for estimating %TBSA burns.
- Lund and Browder chart: This method is commonly used worldwide and accounts for the variation in body shape with age, allowing its use in both adults and children (Figure 3). In infants and small children, the area of the head makes up a larger portion of the total skin area as compared with adults.
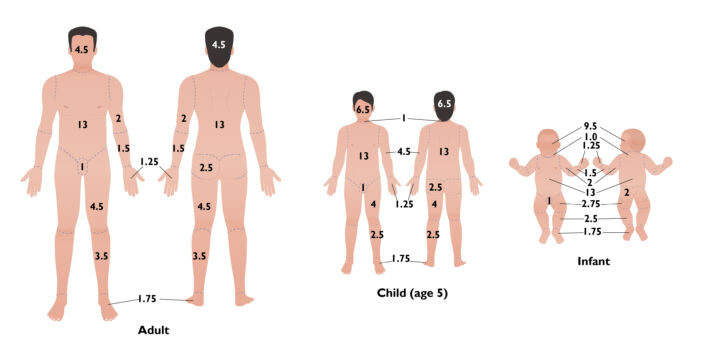
Figure 3. Lund and Browder chart for calculating %TBSA burns.
- Palmar method: In this method, patient’s palm and fingers represent 1% TBSA burns.
- Mortality from burn injuries has improved over the last several decades. In a large analysis, the three risk factors predictive of increased mortality from burns were:1
- age > 60 years;
- > 40% TBSA burns; and
- inhalation injury.
- The mortality rates were 0.3, 3, 33, or 90% depending on whether 0, 1, 2, or 3 risk factors were present.
- Criteria for transfer to a specialized burn center include the following: 2
- >10% partial thickness burns;
- full thickness burns;
- burns involving critical areas (face, hands, genitalia, feet, perineum, crossing joints, etc.);
- circumferential burns;
- electrical and chemical burns;
- inhalation injuries; and
- major preexisting comorbid conditions.
- Mortality from burn injuries has improved over the last several decades. In a large analysis, the three risk factors predictive of increased mortality from burns were:1
Pathophysiologic Changes
- Major burns exceeding 25% TBSA cause a cytokine-mediated inflammatory response that occurs in two phases: a burn shock (ebb) phase during the first 24 to 48 hours that is characterized by a decreased cardiac output and blood flow to all organs, followed by a hypermetabolic (flow) phase at 48 to 72 hours after the initial injury that is characterized by increased O2 consumption, CO2 production, and cardiac output and enhanced blood flow to all organs (Table 2).1,2
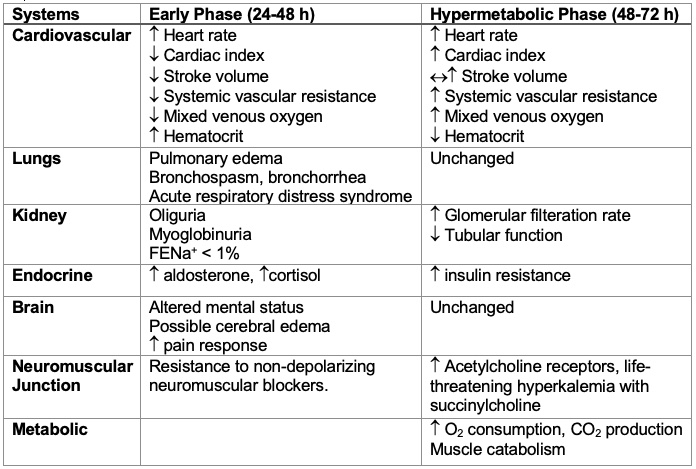
Table 2. Pathophysiological changes following burn injuries. Abbreviation: FENa+ = Fractional extraction of sodium) Adapted from Bittner EA, et al. Anesthesiology. 2015.1
Inhalation Injury
- The presence of inhalation injuries significantly increases the morbidity and mortality.1 The mechanisms of inhalation injuries can be divided into three categories.1,2
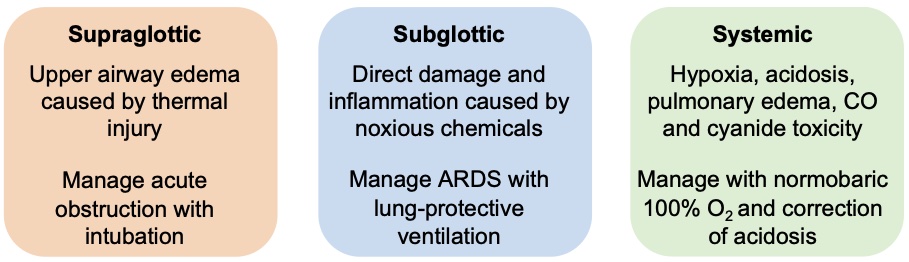
Table 3. Mechanisms of inhalation injuries.
- Carbon monoxide (CO) poisoning presents as altered mental status, nausea, dizziness, and headaches.1,2
- CO binds to hemoglobin with much greater affinity than oxygen, causing the oxygen-hemoglobin dissociation curve to shift to the left.1,2
- Carboxyhemoglobin can be measured through co-oximetry or laboratory studies but cannot be distinguished on standard pulse oximetry.2
- Patients with suspected CO poisoning should receive 100% normobaric O2 which reduces the half-life of CO from 240-320 minutes to 40-80 minutes.2
- In severe cases with carboxyhemoglobin > 20%, consider hyperbaric O2 therapy or intubation and mechanical ventilation with 100% O2.2 The limited availability of hyperbaric O2 centers and logistics of transferring a burn patient to these centers limits its routine use
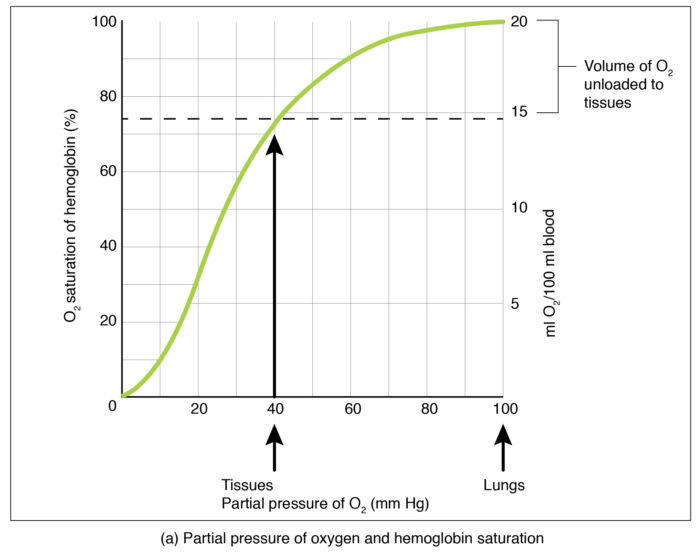
Figure 4. O2-Hgb dissociation curve. Source: Gas Transport CC BY SA 4.0
- Cyanide poisoning can result from toxic gases released from the burning of synthetic materials.
- Cyanide poisoning should be suspected in any patient with smoke inhalation injury with an anion gap metabolic acidosis despite adequate oxygen delivery.1 The patient’s mixed venous oxygen saturation will be elevated.
- Cyanide concentrations greater than 20 ppm are considered dangerous.1
- The treatment of cyanide poisoning is the administration of hydroxocobalamin or the combination of sodium nitrite and sodium thiosulfate.
Airway Management
- Exposure to direct heat can cause upper airway edema and copious secretions leading to acute obstruction.4
- Laryngeal swelling may also be exacerbated by fluid resuscitation.4
- Fiberoptic bronchoscopy is the gold standard for evaluation of erythema, ulceration, and edema in the oropharynx and vocal cords.4
- Early tracheal intubation is recommended in patients with large full-thickness burns, inability to protect the airway, or signs of airway obstruction.5
- The decision of oral versus nasal intubation depends on institutional preference. Some centers prefer nasotracheal intubation because it is easier to secure a nasotracheal tube and it is more comfortable for the patient, especially for a prolonged intubation.
- The awake fiberoptic approach is preferred to maintain spontaneous patient respiration.5
- Neuromuscular blockade with succinylcholine can cause life-threatening hyperkalemia due to delayed upregulation of acetylcholine receptors at 24 to 48 hours after injury.2
- Use of an endotracheal tube 0.5-1 mm smaller than usual allows for laryngeal swelling.4
- Tracheostomy may be preferred in cases of vocal cord damage to prevent further injury.4
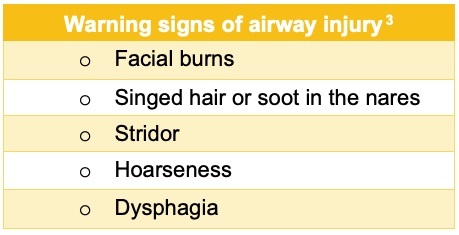
Table 4. Warning Signs of Airway Injury.3
Ventilation
- Patients may develop airway obstruction, bronchospasm, atelectasis, shunt, or acute respiratory distress syndrome leading to decreased compliance.1
- Lung-protective ventilation is the standard of care for burn patients with inhalation injury.1
- Tidal volumes ≤6 mL/kg ideal body weight
- Plateau airway pressures < 30 cm H2O in adults
- Patients with significant inhalation injuries are prone to thick bronchial secretions and casts that predispose them to mucus plugging and complete obstruction of the endotracheal tube. This can result in the emergent need for endotracheal tube exchange and should be considered in acute respiratory decline.
- Circumferential eschars on the chest or abdomen can also cause decreased pulmonary compliance and escharotomy may be necessary.2
- Increased CO2 production during the hypermetabolic state may require higher ventilation rates and even prolonged postoperative mechanical ventilation.2
- Assess readiness for extubation either indirectly with an endotracheal tube cuff leak test, directly with laryngoscopy, or flexible fiberoptic bronchoscopy.2
Fluid Replacement
- Burn shock occurs during the first 24 to 48 hours after a major burn due to intravascular depletion, increased systemic vascular resistance, and decreased cardiac output.5
- Early fluid resuscitation within 2 hours of injury is associated with decreased mortality.2
- Burns < 15% TBSA can be managed with oral or intravenous fluids at 1.5 times maintenance rate.1 For burns > 15% TBSA, multiple fluid resuscitation formulae exist.
- The Parkland formula is most commonly used in the United States, and it recommends isotonic crystalloids initially, and the use of colloids 24h after injury.2
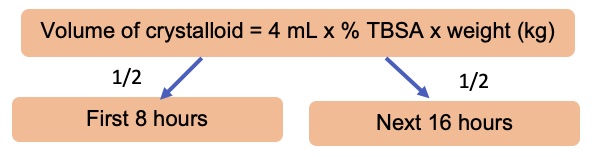
Figure 4. Parkland formula
- Lactated Ringer’s solution is often chosen as the crystalloid secondary to the risk of metabolic acidosis with large volumes of 0.9% normal saline.
- There is controversy regarding the timing of initiation of colloids. Most burn centers initiate colloid administration earlier than the previously recommended 24h after injury.1
- Patients with inhalation injuries require 30-50% more fluid resuscitation.2
- High voltage electrical injuries have an increased fluid requirement up to 9 mL/kg per %TBSA in the first 24 hours,4 with a target urine output of 2 mL/kg/hr.1
- Physiological endpoints of fluid resuscitation in burn patients include:1
- urine output 0.5-1 mL/kg/h;
- blood pressure within normal range;
- central venous pressure 3-8 mm Hg;
- fractional extraction of sodium < 1%;
- blood urea nitrogen/creatinine ratio ≥ 20;
- echocardiogram- normal stroke volume and ejection fraction; and
- base deficit < 5.
Electrical Burns
- Electrical burns are associated with an increased risk of rhabdomyolysis, muscle necrosis, compartment syndrome, and cardiac dysrhythmias.1
- The skin findings of electrical burns can significantly underestimate the degree of internal thermal injury.
- Myoglobinuria secondary to muscle damage may lead to renal tubular injury. Treatment includes the administration of sodium bicarbonate, mannitol, and furosemide to facilitate myoglobin excretion.1
Chemical Burns
- Chemical burns should be irrigated until skin or irrigation fluid pH is neutral by litmus test, with special care taken to avoid irrigation fluid crossing unaffected skin.3
- Some chemicals require specific neutralization agents; thus, rapid identification of the causal agent is key. For example, elemental metals must be irrigated with mineral oil.3
References
- Bittner EA, Shank E, Woodson L, Martyn JAJ. Acute and perioperative care of the burn-injured patient. Anesthesiology 2015; 122:448–464. PubMed
- Hill NE, Mahboobi SK. Anesthesia for patients with burns. In: StatPearls. Published 2022 Jan. Accessed June 2022. Link
- Pardo MC, Miller RD. Anesthesia for Trauma: Burns. In: Basics of Anesthesia. Philadelphia. Elsevier; 2018: 740-2.
- Barash PG, Cullen BF, Stoelting RK, et al. Trauma and Burns. In: Clinical Anesthesia. Philadelphia, PA. Wolters Kluwer; 2017; 32:620-624.
- Wang C. Management of burns and anesthetic implications. Anesthesia for Trauma. 2014;291-319. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.