Copy link
Propofol
Last updated: 08/08/2023
Key Points
- Propofol is an intravenous (IV) anesthetic agent commonly used for the induction and maintenance of general anesthesia, as well as sedation in critically ill patients.
- Propofol exhibits a rapid onset of action, with a duration of 5-10 minutes. This short duration is attributed to its rapid redistribution and metabolism.
- Adverse effects of propofol include dose-dependent hypotension, respiratory depression, pain on injection, and a risk of bacterial growth and contamination due to its lipid emulsion formulation.
Pharmacology
Physiochemical Characteristics
- Propofol (2,6-diisopropylphenol) is available as a lipid-based emulsion formula containing soybean oil, glycerol, and purified egg phosphatide.
- Propofol is an insoluble drug. Current formulations use soybean oil as the oil phase, and egg lecithin as the emulsifying agent.
- Diprivan® brand formulation uses disodium edentate as a preservative, along with sodium hydroxide to achieve a pH of 7 to 8.5.
- The generic formulation of propofol uses sodium metabisulfite as a preservative, with a pH of 4.5 to 6.4.
Mechanism of Action1
- Propofol acts by enhancing the inhibitory effects of gamma-aminobutyric acid (GABA) through its interactions with GABAA receptors, which are ligand-gated chloride channels, in the central nervous system (CNS).
- Propofol binds to specific sites on GABAA receptors, located at the interface between the α and β subunits.
- The binding of propofol to these receptors potentiates the inhibitory actions of GABA by increasing the duration of GABA-activated channel opening. This leads to increased chloride influx and hyperpolarization of postsynaptic neuronal membranes, resulting in inhibition of postsynaptic neurons, and subsequent sedation and anesthesia.
- Propofol has a rapid onset of action due to its high lipid solubility.
- Propofol’s lipophilic nature also facilitates its rapid penetration of the blood-brain barrier, allowing for efficient action at CNS sites.
Pharmacokinetics1
- The pharmacokinetics of propofol are listed in Table 1.
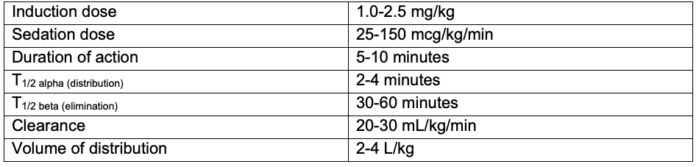
Table 1. Pharmacokinetics of propofol
- Redistribution:
- Propofol has a very short initial distribution half-life (2-4 minutes). It undergoes rapid redistribution from the brain and other highly perfused tissues into less well perfused tissues (e.g., muscle, fat). This explains the rapid recovery from a single bolus dose for the induction of anesthesia.
- Propofol’s long elimination half-life is related to its slow diffusion from the poorly perfused, lipophilic peripheral compartment (e.g., muscle, fat) into the central compartment. After a prolonged administration, even though a large amount of propofol remains in the peripheral compartment, rapid and extensive metabolism of propofol that slowly diffuses into the central compartment causes its concentration to decline below the hypnotic threshold, resulting in awakening. Propofol’s context-sensitive half time is less than 40 minutes even for propofol infusions lasting up to 8 hours.
- Metabolism:
- Propofol undergoes extensive hepatic metabolism. The primary metabolic pathways involve glucuronidation and oxidation.
- Conjugation with glucuronic acid results in the formation of inactive metabolites.
- Excretion:
- Propofol and its metabolites are primarily eliminated through the renal route, predominantly via urine.
- Approximately 90% of the administered propofol dose is excreted within 24 hours, mainly as glucuronide conjugates.
- Protein Binding:
- Propofol exhibits high-protein binding, with approximately 95% bound to plasma proteins.
- Children and Elderly patients
- Children require higher induction and maintenance doses of propofol (on a per kg body weight basis) secondary to a larger central distribution volume and higher clearance rate.
- Elderly patients require lower induction and maintenance doses of propofol as a result of their smaller central distribution volume and decreased clearance rate.
- Route of Administration and Bioavailability:
- IV route:
- Propofol possesses 100% bioavailability when administered intravenously.
- Onset of action is rapid, typically occurring within 1 minute.
- IV route:
Systemic Effects
The systemic effects of propofol administration are listed in Table 2.
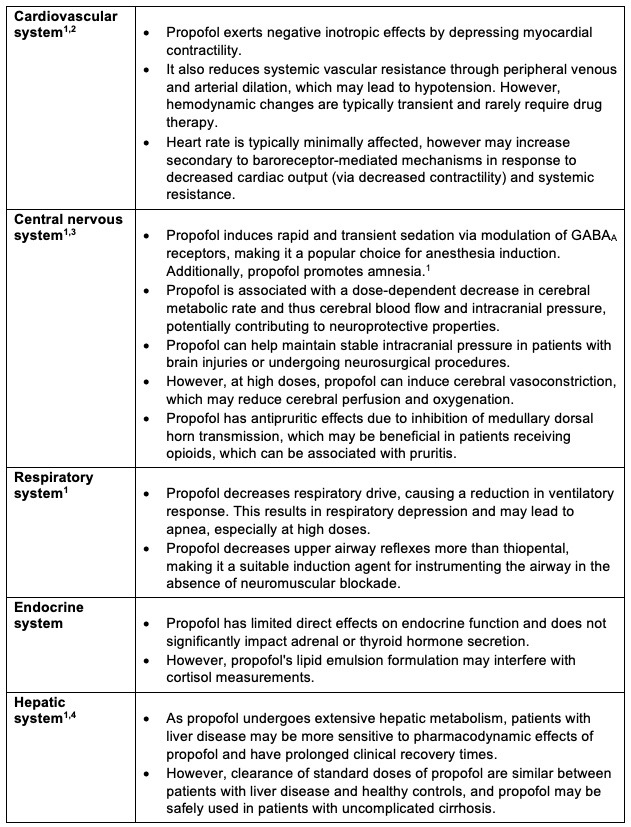
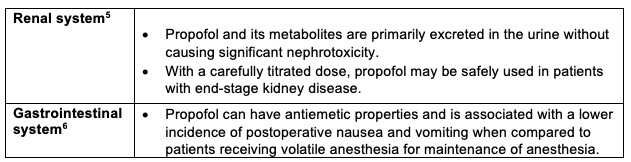
Table 2. Systemic effects of propofol administration
Propofol Infusion Syndrome7
- Propofol infusion syndrome (PRIS) is a rare but potentially fatal condition associated with prolonged high-dose propofol infusion.
- PRIS manifests as metabolic acidosis, rhabdomyolysis, hyperkalemia, lipidemia, and cardiac dysfunction.
- The pathophysiology of PRIS is not fully elucidated but likely involves mitochondrial dysfunction and impaired fatty acid metabolism.
- PRIS primarily affects pediatric patients but can also occur in adults, especially those receiving prolonged high-dose propofol infusions.
- Routine biochemical monitoring of triglycerides, serum lactate, creatinine kinase, and myoglobin throughout a propofol infusion may facilitate early identification of PRIS.
Clinical Uses8,9
Induction and Maintenance of General Anesthesia
- Propofol is the most common induction agent for general anesthesia due to its rapid onset, smooth pharmacokinetics, and favorable recovery profile.
- Continuous infusion or intermittent bolus administration of propofol can be employed for the maintenance of general anesthesia, ensuring precise control over the depth of anesthesia throughout the surgical procedure.
Sedation for Medical Procedures
- Propofol is widely employed for procedural sedation, particularly in endoscopic procedures, bronchoscopy, and interventional radiological interventions.
- Its rapid onset, short duration of action, and ability to provide profound sedation make it advantageous for achieving optimal patient comfort and cooperation during these procedures.
- The modulation of GABAA receptors by propofol contributes to its sedative effects, with concurrent induction of amnesia, minimizing patient recall of the procedure.
Sedation in Monitored Anesthesia Care (MAC)
- Propofol is also utilized for sedation in the context of monitored anesthesia care (MAC), wherein patients receive local anesthesia, analgesia, and sedation during various surgical or diagnostic procedures.
- It allows for precise titration of sedation levels, ensuring optimal patient comfort, cooperation, and analgesia while maintaining the ability to communicate and respond appropriately.
Sedation in Intensive Care Units (ICUs)
- Propofol finds extensive application for sedation in critically ill patients, particularly those requiring mechanical ventilation or recovering from major surgical procedures in the ICU.
- Its rapid onset and favorable pharmacokinetics allow prompt titration to achieve the desired level of sedation and optimize patient-ventilator synchrony through its respiratory depressive effects.
- The CNS depressant effects of propofol alleviate anxiety, promote patient comfort, and facilitate the management of ventilatory support.
Treatment of Refractory Status Epilepticus
- Propofol serves as an adjunctive therapy in the management of refractory status epilepticus, a severe condition characterized by prolonged or recurrent seizures unresponsive to initial antiseizure medications.
- Its potent GABAergic activity leads to profound CNS depression, terminating seizures and restoring normal brain activity.
- IV propofol infusion, guided by continuous electroencephalogram (EEG) monitoring, is employed in a closely monitored setting to ensure precise titration and minimize the risk of adverse events.
Adverse Effects
- Propofol’s most significant adverse effect is dose-depending hypotension. Systolic blood pressure has been shown to decrease to less than 90 mmHg in 16 percent of patients.2
- While this hypotension is typically transient, propofol should be used with caution in patients who are hypovolemic, have preexisting hemodynamic compromise, or are elderly.
- Propofol may also cause a dose-dependent respiratory depression, with consequence decrease in respiratory rate, tidal volume, and ventilatory responses to hypoxia and hypercapnia, and apnea.
- Propofol causes pain on IV injection in many patients, especially in smaller veins, and thus, is typically coadministered with lidocaine or an opioid.
- Due to the lipid emulsion containing egg lecithin, glycerol, and soybean oil, propofol supports bacterial growth and is associated with contamination risk, fever, infection, and sepsis.10
- Allergic reactions to propofol are rare, even in patients with pre-existing egg, peanut, or soy allergies. A history of egg allergy does not contraindicate the use of propofol since most egg allergies are to albumin in the egg white, whereas egg lecithin is extracted from egg yolk.
Propofol Derivatives
- Propofol derivatives are chemically modified versions of the original drug propofol.
- These derivatives are designed to maintain or enhance the desirable properties of propofol while reducing its side effects or improving its pharmacokinetic profile.
- The safety and efficacy of these derivative drugs are under investigation in clinical trials.
PFO7131
- PFO713 is a propofol derivative with larger side chains at the 2 and 6 positions on the phenol ring.
- Like propofol, PFO713 is a potent GABAA receptor potentiator, inducing reliable anesthesia.
- Compared to propofol, PFO713 has an improved cardiovascular side-effect profile.
Fospropofol1
- Fospropofol is a pro-drug of propofol. It converts to the active form within minutes of IV injection.
- Compared to propofol, fospropofol has a delayed onset of action and a slower recovery.
- Fospropofol is not associated with pain on injection; however, it may cause perineal pain or paresthesia.
References
- Khan KS, Hayes I, Buggy DJ. Pharmacology of Anaesthetic Agents I: intravenous anaesthetic agents. Continuing Education in Anaesthesia Critical Care & Pain. 2014:14(3): 100-5. Link
- Hug CC Jr, McLeskey CH, Nahrwold ML, et al. Hemodynamic effects of propofol: data from over 25,000 patients. Anesth Analg. 1993; 77(4): S21-9. PubMed
- Kotani Y, Shimazawa M, Yoshimura S, et al. The experimental and clinical pharmacology of propofol, an anesthetic agent with neuroprotective properties. CNS Neurosci Ther. 2008;14(2):95-106. PubMed
- Servin F, Desmonts JM, Haberer JP, et al. Pharmacokinetics and protein binding of propofol in patients with cirrhosis. Anesthesiology. 1988;69(6):887-91. PubMed
- Ickx B, Cockshottt ID, Barvais L, et al. Propofol infusion for induction and maintenance of anaesthesia in patients with end-stage renal disease. Br J Anaesth. 1998;81(6):854-60. PubMed
- Gan TJ, Belan KG, Bergese S, et al. Fourth consensus guidelines for the management of postoperative nausea and vomiting: Erratum. Anesth Analg. 2020; 131(2): 411-48. PubMed
- Riker RR, Glisic EK Fraser GL. Propofol infusion syndrome: Difficult to recognize, difficult to study. Critical Care Medicine. 2009; 37(12):3169-70. PubMed
- Ho KM, Ng JY. The use of propofol for medium and long-term sedation in critically ill adult patients: A meta-analysis. Intensive Care Med. 2008; 34(11):1969–79. PubMed
- White PF. Clinical uses of intravenous anesthetic and analgesic infusions. Anesth Analg. 1989; 68(2):161–71. PubMed
- Muller AE, Huisman I, Roos PJ, et al. Outbreak of severe sepsis due to contaminated propofol: Lessons to learn. J Hosp Infect. 2010; 76(3): 225–30. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.