Copy link
Perioperative Sinus Bradycardia
Last updated: 04/26/2023
Key Points
- Sinus bradycardia, commonly defined as sinus rhythm below 60 beats per minute (bpm), normally occurs in children and adults during sleep and in well-conditioned athletes.
- Sinus bradycardia is the most common bradyarrhythmia during anesthesia and surgery and can also occur in several pathological states.
- Hypoxemia is the most common cause of sinus bradycardia and cardiac arrest in children.
- Patients with symptomatic sinus bradycardia should be promptly treated.
- Heart transplant patients with bradycardia should be treated with direct sympathomimetic agents such as isoproterenol and epinephrine.
Introduction
- Bradycardia in adults is defined as sinus rhythm below 60 beats per minute (bpm).1 In children, the normal range for heart rate varies with age, and bradycardia is defined as an awake heart rate below 100 bpm in infants, 80 bpm in toddlers and young children, 70 bpm in school-aged children, and 60 bpm in adolescents.2
- Sinus bradycardia is essentially sinus rhythm at a rate below 60 bpm (Figure 1).1 Sinus bradycardia is the most common bradyarrhythmia during anesthesia and surgery.3
- The cardiac impulse originates in the sinus node and spreads to the atrioventricular (AV) node and through the atria, resulting in atrial contraction. From the AV node, the impulse spreads to the bundle of His and bundle branches, resulting in ventricular contraction.
- Both the parasympathetic and sympathetic nervous systems affect the heart rate. Increased parasympathetic tone decreases the pacing rate of the sinus node and slows AV conduction resulting in a reduced heart rate, and increased sympathetic tone increases sinus node pacing resulting in an increased heart rate.
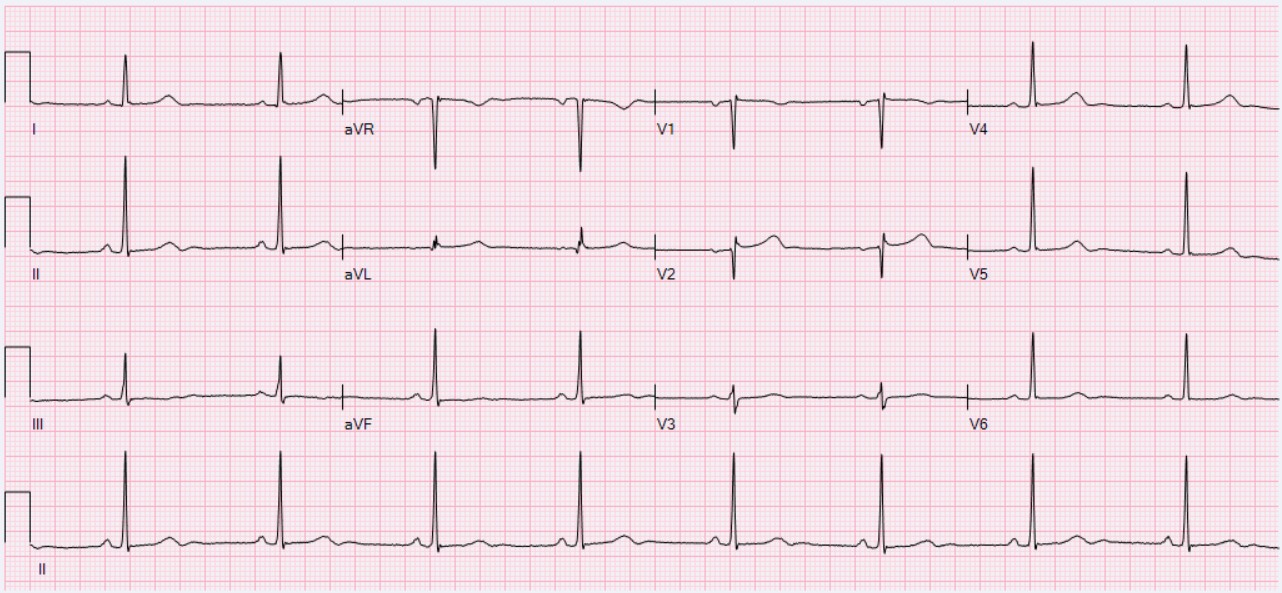
Figure 1. Sinus bradycardia with a heart rate of 49 bpm. Source: Wikimedia Commons. Ewingdo. CC BY-SA 4.0. Link.
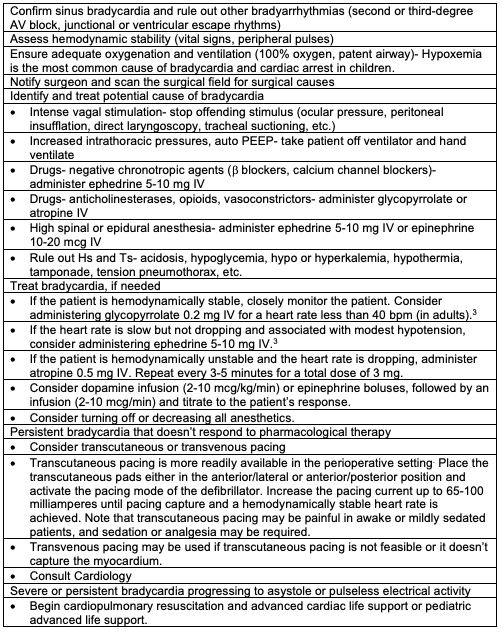
Table 1. Management of perioperative sinus bradycardia. Adapted from Methangkool E, Mahajan A. Arrhythmias during anesthesia. In: Post T, ed. UpToDate; 2023. Accessed February 18th, 2023. Link.
- The American Heart Association (AHA) guidelines for managing adults with bradycardia can be accessed here (Link).6
- The AHA guidelines for pediatric bradycardia with a pulse can be accessed here (Link) and includes the following recommendations.7
- The airway should be assessed and supported first, and then assess the circulation (ABC).
- Chest compressions should be started for a heart rate of less than 60 bpm despite adequate oxygenation and ventilation.
- Epinephrine should be administered for unstable bradycardia (see below for when to use atropine) at a dose of 0.01 mg/kg (0.1 mL/kg of the 0.1 mg/mL concentration) IV and repeat every 3-5 minutes. The maximum single dose of epinephrine is 1 mg.
- Atropine should be administered for patients with increased vagal tone or primary AV block at a dose of 0.02 mg/kg IV and repeated once, if necessary. In children, the minimum dose of atropine is 0.1 mg, and the maximum dose is 0.5 mg.
- Reversible causes of bradycardia, such as hypoxemia, head injury, toxins, and increased vagal tone should be identified and treated.
- If bradycardia persists, transcutaneous or transvenous pacing should be considered.
Bradycardia and Heart Transplant
- Patients with heart transplants have denervation of the heart and will not respond to indirectly acting agents such as ephedrine and anticholinergics.
- Therefore, bradycardia in these patients should be treated with direct sympathomimetic agents such as isoproterenol or epinephrine.
References
- Homoud MK. Sinus bradycardia. In: Post T, ed. UpToDate; 2023. Accessed February 18th, 2023. Link
- Silva JN. Bradycardia in children. In: Post T, ed. UpToDate; 2023. Accessed February 18th, 2023. Link
- Methangkool E, Mahajan A. Arrhythmias during anesthesia. In: Post T, ed. UpToDate; 2023. Accessed February 18th, 2023. Link
- Steyn J, Dorfling J. Sinus bradycardia. In: Gaba, DM, Burden AR, Howard SK, Fish KJ. Crisis Management in Anesthesiology. 2nd Edition. Philadelphia, PA. Elsevier/Saunders; 2015: 160-3.
- Kuan C, Pukenas EW. Bradycardia in the pediatric patient. In: Gaba, DM, Burden AR, Howard SK, Fish KJ. Crisis Management in Anesthesiology. 2nd Edition. Philadelphia, PA. Elsevier/Saunders; 2015: 364-8.
- Panchal AR, Bartos JA, Cabańas JG, et al. Part 3: Adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142: S366-468. PubMed
- Topjian AA, Raymond TT, Atkins D, et al. Part 4: Pediatric basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142: S469-523. PubMed
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.